Caring for a baby at night is a tender, tiring dance. If you’re reading this after a long stretch of wake-ups, I’m right there with you. As a gentle parenting advocate and seasoned mom, I’ve walked parents through the bleary hours and found that a steady mix of responsive care, realistic expectations, and evidence-based strategies turns the night from a battleground into a rhythm. Below, I’ll help you understand what’s normal, what’s fixable, and how to choose the right tools and methods for your family—especially if you’re breastfeeding, healing postpartum, or selecting safe baby gear, including a baby sleep sound device that can help soothe your baby to sleep.
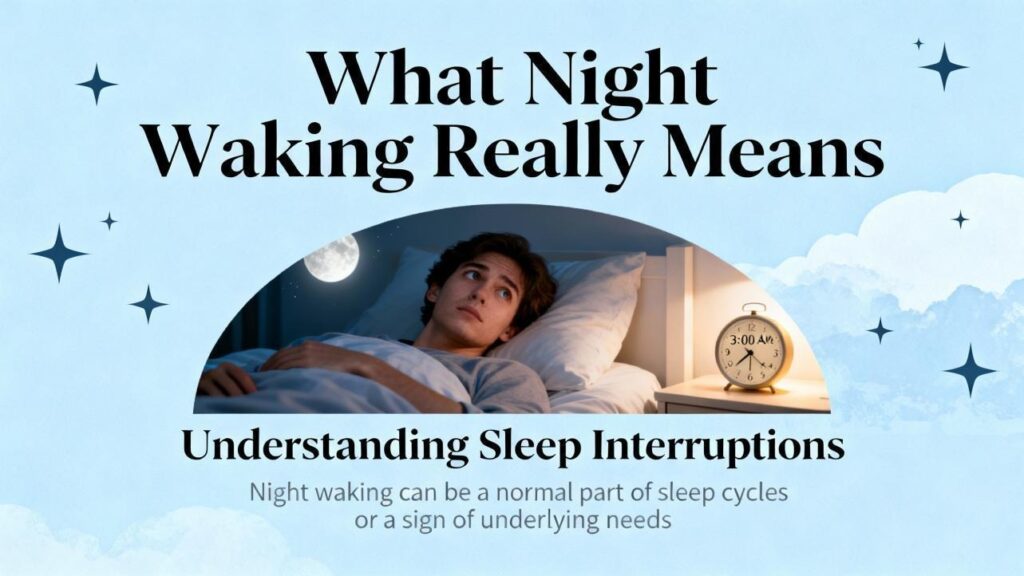
What Night Waking Really Means
Most babies wake briefly multiple times overnight as they transition between sleep cycles. Waking four to six times and then resettling is common across infancy and even in adulthood. “Sleeping through the night” isn’t a single universal milestone. Many clinical and parent resources define it as about six uninterrupted hours without calling out, while some parenting programs reserve the phrase for a 10–12 hour stretch without caregiver help. The practical takeaway is kinder: your baby is progressing when their brief arousals increasingly end with them drifting back to sleep on their own.
Newborns wake frequently because they need to eat. Around the early weeks, they may feed eight to twelve times per day and continue overnight. Once a baby is growing well and your pediatrician or lactation consultant clears longer stretches, many infants begin consolidating sleep. By around six months, a sizable portion can physiologically manage longer stretches without feeding, although many still wake. It’s also normal to see a spike in wakefulness near three to four months as sleep architecture matures; this is the well-known “four‑month regression,” which is really a developmental progression that increases sensitivity to environment and sleep associations.
Behavioral insomnia of childhood, as described by the American Academy of Sleep Medicine, often looks like trouble falling asleep without a specific help cue (for example, feeding, rocking, or being held) or escalating bedtime negotiations that spill into the night. The good news: research shows that consistent, age‑appropriate behavioral strategies are effective and safe when implemented thoughtfully, and many families see improvements within one to two weeks. Benefits tend to last when routines are maintained.
Before You Problem‑Solve: Rule Out Health or Feeding Issues
When frequent waking becomes all‑night wakefulness, a brief assessment is worthwhile. A focused sleep history and a simple diary for a few days can reveal patterns. Consider hunger patterns, reflux discomfort, eczema itch, pain, snoring or mouth breathing, and recent changes such as vaccines, travel, illness, or teething. Pediatric sources recommend calling your clinician promptly if wake‑ups are hourly all night, there are concerns about weight gain or breathing, reflux signs are prominent, or your instincts tell you something is off.
For breastfed babies, the best day‑to‑day adequacy checks are weight trajectory, six or more wet diapers in 24 hours after the first week, and contentment after feeds. If wakes cluster despite robust daytime feeding, ask your pediatrician or lactation consultant about optimizing daytime calories, timing feeds, and whether a late‑evening “dream feed” fits your situation. If formula feeding, review volume and spacing to avoid daytime “snacking” that shifts calories to the night.
Foundations That Make the Biggest Difference
Circadian rhythm and schedule fit
Sleep is easier when wake time pressure is right. Age‑appropriate “wake windows” are practical guardrails: newborns often do best with 30 minutes to 2 hours awake between sleep periods, while older infants commonly tolerate 2.5 to 3.5 hours by late infancy, with the shortest wake window before the morning nap and the longest before bedtime. When windows are too short, babies may not be sleepy. When they are too long, cortisol rises, bedtime tears escalate quickly, and wake‑ups multiply. If your baby falls asleep in under five minutes at bedtime or melts down rapidly, that’s often a sign of overtiredness; trim the final wake window or protect naps. Morning daylight, engaging play during wake times, and dimming lights at least an hour before bed help align the body clock.
Bedtime routine and sustainable sleep associations
A short, predictable routine teaches your baby that sleep is coming. Many families use some version of bath, feed, a brief story or lullaby, and lights out. The order matters less than consistency and keeping stimulation low. Putting your baby down drowsy but awake is a skill‑builder. It reduces dependence on a particular sleep onset association—like nursing to sleep, being rocked, or holding a pacifier in place—and gives your baby practice falling asleep in the same environment they’ll experience between cycles at night. As early as around three months, a gentle pick‑up/put‑down approach can help: soothe in arms until calm, then lay down drowsy; if fussing returns, pause briefly, then pick up to calm again, repeating with gradually longer pauses over several nights.
Sleep environment tweaks that pay off
Babies tend to sleep better in a cool, dark, quiet space. Pediatric guidance commonly targets a room temperature around 68–72°F. Blackout shades reduce early wakes, and steady white noise can mask household and street sounds. If you use a sound machine, place it about seven feet from the crib and keep the volume modest—no higher than conversational levels. Keep lighting and sounds consistent from bedtime through the night; a dark, boring night signals “time to sleep,” not “time to practice standing.”
Gentle responsiveness without reinforcing wakefulness
A brief pause before responding lets you differentiate between a between‑cycle murmur and a true need. If your baby starts to resettle, allow it. If they need help, offer the least assistance that works: shushing, a gentle hand on the chest, rhythmic patting, or a calm voice while they remain in the crib. With consistency, this “minimal effective comfort” supports attachment and learning. Trust your instincts; if your baby’s cry changes or your gut flags discomfort, respond and reevaluate.
Evidence‑Based Behavioral Strategies, Compared
Professional organizations synthesize a wide range of studies on infant sleep. The American Academy of Sleep Medicine highlights several behavioral strategies—unmodified extinction, graduated extinction, bedtime fading, positive routines, and scheduled awakenings—that reduce sleep onset delay and night wakings, with no evidence of harm to attachment when done appropriately. Families do best when they choose an approach that matches their values and their baby’s temperament, and then apply it consistently for at least a week unless illness or travel intervenes.
| Method | What it is | Best for | Pros | Considerations |
|---|---|---|---|---|
| Unmodified extinction | Bedtime routine, then place baby down awake and do not re‑enter until a set morning time or a planned feed | Families comfortable with low‑intervention plans; babies older than the newborn phase cleared for longer stretches | Often rapid results over a few nights; clear expectations | Can be emotionally hard for caregivers; not a fit for every family’s philosophy |
| Graduated extinction | Similar to above, but with timed, brief check‑ins that are soothing yet minimal | Families wanting incremental steps and some presence | Evidence‑based and flexible; maintains consistency | Requires tracking intervals; check‑ins can stimulate some babies |
| Bedtime fading | Temporarily set bedtime later to match natural sleep onset, then shift bedtime earlier by small increments | Babies who resist bedtime or take very long to fall asleep | Reduces bedtime battles by leveraging sleep pressure | Requires careful observation and may take longer to see results |
| Positive routines | Build a consistent, enjoyable, short routine before lights out; reinforce calm behaviors | Younger infants and families focusing on foundations first | Low stress, supports attachment and predictability | Works best combined with drowsy‑but‑awake and a consistent response plan |
| Scheduled awakenings | Preemptively wake and soothe just before habitual wakings, then gradually reduce | Predictable, clock‑like night wakings | Helpful for pattern “resetting” | Requires night tracking and time‑limited use |
Some resources raise concerns about stress physiology during certain training methods. For example, analyses summarized by BASIS discuss studies where crying decreased but infant cortisol remained elevated early on. At the same time, pediatric sleep organizations and reviews report no evidence of harm to attachment from behavioral strategies when used appropriately and consistently. Reconciling these views, I encourage families to choose the least‑intense method they can apply consistently, to pause for illness or travel, and to monitor their own mental well‑being alongside their baby’s cues.
Breastfeeding, Night Weaning, and Protecting Milk Supply
Feeding patterns and sleep are intertwined. In the early weeks, frequent night feeds are normal and important for growth and milk supply. As intake increases and your clinician clears longer stretches, consolidating calories into daytime helps reduce hunger‑driven wakes. If a baby takes most calories overnight, that “reverse cycling” can sustain wakes; offering fuller, more frequent daytime feeds and gently spacing night feeds can help. Some families find that a late evening dream feed—offered around 10:00–11:00 PM while keeping lights low and interactions quiet—extends the first stretch of night sleep.
Because breastfeeding supply responds to removal, it’s important to pair gradual night weaning with daytime feeding support. For a breastfed baby still needing a night feed, nursing one side overnight while prioritizing both sides during the day is one approach some pediatric sources discuss; confirm with your clinician or lactation consultant to protect supply and your baby’s growth curve. Signs that hunger is not the primary driver of wakes include brief wake times without robust feeding, predictable same‑time wakes unrelated to daytime intake, and quick resettles with non‑feeding soothing.
Safe Baby Gear That Truly Helps
The safest sleep surface remains a firm, flat mattress in a safety‑approved crib or bassinet with no soft items. Many pediatric and hospital sources recommend room‑sharing (but not bed‑sharing) for the first several months. If swaddling helps your newborn sleep, keep hips able to move freely and transition out of swaddles at the first signs of rolling, moving to a wearable sleep sack to maintain warmth without loose bedding. A well‑chosen sound machine and good blackout curtains can reduce environmental triggers for wakes. Consumer wearables and video monitors can offer peace of mind, but clinical sources caution that physiologic monitoring remains a specialized tool; prioritize safe‑sleep practices over numbers on a screen and consult your pediatrician about any medical concerns.
| Item | What to look for | Care tips | Watch‑outs |
|---|---|---|---|
| Crib and mattress | Slats no more than about 2 and 3/8 inches apart; firm, flat, well‑fitting mattress and sheet | Check hardware periodically; keep the sleep space clear | Avoid pillows, bumpers, positioners, and soft toys in the crib |
| Swaddle and sleep sack | Hip‑healthy designs; secure closures that cannot unravel; correct size | Stop swaddling at first roll; wash per fabric instructions | Do not swaddle once rolling; avoid overheating by dressing lightly underneath |
| White noise machine | Continuous, non‑looping sound; volume control with clear decibel markings; ability to set a low volume | Place roughly seven feet from the crib; use the lowest effective volume | Keep volume no louder than a normal conversation; avoid placing on the crib |
| Blackout solution | Truly light‑blocking curtains or shades; safe installation | Keep cords safely tucked away; ensure ventilation | Avoid bright nightlights that can cue wakefulness |
| Wearables/monitors | Clear purpose (video for observation; not medical); secure fit and safe materials | Follow manufacturer guidance; check for skin irritation | Do not treat consumer devices as medical monitors; discuss concerns with your pediatrician |
Gentle Parenting in Practice: Responding at Night Without Reinforcing Wakefulness
Gentle parenting at night means staying responsive while guiding toward independent sleep. A helpful sequence is to pause briefly, listen, and decide whether your baby is practicing a new skill, lightly fussing, or asking for help. If soothing is needed, begin with in‑crib comfort like a calm voice and a hand on the chest. If that falls short, pick up to calm, then lay back down drowsy; repeat with steady, unhurried confidence. Keep nights dim and quiet, save playful chatter for daytime, and preserve your routine even during regressions. Consistency is the gift that makes gentle approaches work.
Special Situations: Regressions, Teething, Travel, and Illness
Near three to four months, sleep becomes more adult‑like with lighter stages and distinct cycles, which can increase wakes if sleep associations are strong. Developmental bursts, like rolling, pulling to stand, or practicing new words, also create temporary bumps. Teething can nudge wakes for some babies. In these phases, protect naps to prevent overtiredness, maintain your routine, offer extra comfort, and keep your response pattern consistent. For predictable, same‑time wakes, scheduled awakenings for a few nights can break the pattern, then taper. During illness or travel, prioritize comfort and hydration, then “reset” with your usual routine once your baby is well and home.
What Research Says—and Where It Disagrees
Large practice parameters and children’s hospital guidance consistently recommend behavioral strategies and strong sleep hygiene as first‑line approaches for bedtime problems and night wakings. Many families see improvements in one to two weeks, with benefits maintained at three to six months when routines are reinforced. There is no evidence that behavioral sleep strategies harm attachment when used thoughtfully and developmentally appropriately. At the same time, some research summarized by infant sleep information groups raises thoughtful questions about stress biology early in training. The most balanced view is this: align on a plan that fits your family’s values, choose the least‑intense method you can sustain, attend to feeding adequacy and medical needs first, and check in with your pediatrician if progress stalls.
Two Real‑World Roadmaps
When I support a four‑month‑old waking every one to two hours, the path begins with feeding adequacy and daytime calories, then right‑sizing wake windows to prevent overtiredness, sharpening a short bedtime routine, and practicing drowsy‑but‑awake with brief in‑crib soothing. For parents who want more structure, a graduated check‑in plan with set intervals often helps. A white noise machine placed about seven feet away at a low volume and true darkness in the sleep space reduce between‑cycle arousals that turn into wakes.
For a nine‑month‑old waking at the same times nightly, I look for habit wakes and reverse cycling. We shift calories into the day with full, predictable feeds, keep naps age‑appropriate, and decide on either scheduled awakenings for a few nights or bedtime fading if falling asleep is the main struggle. If one night feed remains appropriate, we keep it brief, calm, and at roughly the same time, then wean gradually with your clinician’s support. Consistency turns the corner.
Postpartum Well‑Being and Partnering at Night
Your rest matters. Research connects parental sleep loss with mood challenges, and the flip side is true: when nighttime patterns improve, caregiver well‑being often follows. Trade early‑evening coverage with a partner, use weekend “sleep‑in” shifts, and accept help for meals or chores. If you’re breastfeeding, a partner can handle the bedtime routine or the diaper and resettle, while you focus feeds during the day and at any clinically appropriate night feed. If persistent low mood, anxiety, or intrusive thoughts appear, reach out to your healthcare team. You deserve support as much as your baby does.
Quick Reference: Methods and When They Shine
While there is no single “right” way, certain approaches align well with particular problems. Graduated check‑ins suit families who want presence with structure. Bedtime fading is smart when a baby takes an hour to fall asleep. Positive routines and in‑crib soothing are perfect for younger infants and gentle parenting preferences. Scheduled awakenings are a precise tool for clock‑like wakes. Full extinction can be effective for some families prepared for a short period of protest. Across all methods, consistency is the engine of change.
FAQ
When should I expect my baby to sleep through the night?
It depends on how you define it. Many pediatric and research sources consider six uninterrupted hours without signaling to be sleeping through the night. Others use 10–12 hours without caregiver help. Newborns wake to eat, and many babies consolidate longer stretches once they are growing well and cleared by a clinician. By around six months, many can manage longer stretches, though a notable portion still wakes and resettles.
Will responding quickly at night “spoil” my baby?
No. Briefly pausing to listen and then responding with the least help needed supports both attachment and learning. What maintains wakefulness is inconsistent patterns or strong sleep‑onset associations that the baby cannot reproduce independently. Calm, predictable routines and in‑crib soothing help you remain responsive without reinforcing full wake‑ups.
Is sleep training safe for attachment?
Reviews from pediatric sleep organizations report no evidence of harm to attachment when behavioral strategies are used appropriately and developmentally. Some research groups highlight early stress markers during more intensive methods; that’s one reason to choose an approach you can apply calmly and consistently, pause for illness, and monitor how your baby responds. If a method feels wrong for you, pick a gentler one.
How do breastfeeding and night weaning fit together?
In the early weeks, night feeds support growth and milk supply. As intake grows and your pediatrician or lactation consultant clears longer stretches, shifting calories into the day helps reduce hunger‑driven wakes. Gradual night weaning, coupled with robust daytime feeding and continued responsive care, protects supply and your baby’s weight trajectory. Personalized guidance from a lactation consultant is invaluable here.
Do white noise machines and blackout curtains really help?
They can. White noise masks disruptive sounds, and darkness cues melatonin and reduces early wakings. Place the sound source about seven feet from the crib and keep volume modest. Blackout solutions work best when they truly block stray light. These tools won’t fix a schedule mismatch or a strong sleep‑onset association by themselves, but they amplify the benefit of your routine and response plan.
When should I call the pediatrician?
Reach out if wake‑ups are hourly all night, your baby shows signs of discomfort or breathing difficulty, there are concerns about weight gain or reflux, or your instincts say something isn’t right. Also call for sudden, persistent changes in sleep not explained by hunger, schedule shifts, or the usual developmental bumps.
Takeaway
Nighttime wakefulness becomes more manageable when you combine realistic expectations, a right‑sized schedule, a soothing routine with drowsy‑but‑awake practice, a calm environment, and a response plan you can sustain. Evidence‑based strategies—from gentle pick‑up/put‑down to graduated check‑ins or bedtime fading—are tools in your toolbox, not tests of your parenting. Feed well in the day, protect naps, choose safe gear, and take care of yourself. Progress often appears within one to two weeks and holds when routines do. Your baby’s sleep story is a journey, and with a compassionate, consistent approach, your nights can become steadier and far more restful.
Sources cited in text include guidance and research from the American Academy of Sleep Medicine, HealthyChildren.org (American Academy of Pediatrics), Nationwide Children’s Hospital, Sleep Foundation, Mayo Clinic, Johns Hopkins Medicine, Huckleberry, What to Expect, and BASIS (Baby Sleep Information Source).